Image-enabling the Electronic Medical Record (EMR) is generally the last step in providing the clinician with access to the patient’s complete Medical Record. The EMR itself is reasonably capable of managing and displaying the discrete data about the patient such as that data forwarded by measuring or monitoring devices, the medication list, documented allergies, etc. An Enterprise Content Management (ECM) solution is the ideal way to manage the unstructured data associated with the patient such as scanned documents, diagnostic reports, lab results, care summaries…the non-image data. This unstructured data is easily accessed and displayed through a link from the EMR to the ECM solution. Accessing and displaying the structured data associated with the patient, the medical images, has historically been more problematic.
Until recently, accessing and displaying the patient’s radiology and cardiology studies was reasonably straightforward. The clinicians would directly access and launch the clinical display application associated with the radiology or cardiology PACS. Alternatively those images being managed by a PACS could be accessed through the EMR by invoking a link to the studies associated with the radiology report being displayed by the EMR. Unfortunately there are number of problems with this approach to accessing/display a patient’s medical images.
- The clinician has to learn and remember how to use multiple viewing applications.
- Each display application is limited to displaying only those images being managed by that PACS. There is generally no way to display images from different imaging departments (radiology and cardiology) on the same screen at the same time. This means the clinician has to bounce back and forth between two viewers to display disparate studies related to a single episode of care.
- PACS-based imaging studies represent a fraction of the medical images that belong in the patient’s complete Medical Record. There are imaging studies in other departments like Endoscopy and Ophthalmology that are not yet being managed by a PACS. There are also all of those non-DICOM images that are being managed on mobile devices and PC’s.
The strategy for image-enabling the EMR should include a methodology and timetable for accessing the DICOM images (studies being managed in PACS and non-PACS scenarios), as well as what I refer to as the “informal images”, those images that are typically acquired in non-DICOM data formats like JPEG and MPEG. Examples include: [1] a series of JPEG images representing a burn wound that were captured by a digital camera or iPhone in the burn unit, [2] a series of JPEG images illustrating a skin rash that were captured during a series of dermatology office visits, [3] a series of MPEG clips taken during visits to the podiatry clinic representing the patient’s gate with and without the orthotic appliance. All of these imaging examples are clinically relevant to the patient, whether there is an associated formal report based on those images or not, and they rightfully belong in the patient’s complete Medical Record.
Current generation department PACS are focused on a specific imaging department. They can acquire, manage and display most DICOM objects, therefore DICOM imaging studies, and the features and functions of the display are customized for the type of studies performed in that department. These PACS typically do not handle non-DICOM image objects unless they are wrapped with a DICOM header and are associated with an existing DICOM study. Department PACS typically do not handle imaging studies comprised solely of non-DICOM image objects. These inherent limitations of the current generation of PACS is the major reason why the UniViewer (universal image viewer) was developed to image-enable the EMR.
There are a number of commercially available UniViewers that can accept and display non-DICOM images, but in many cases those images once again have to be wrapped with a DICOM header and associated with an existing DICOM study (added to the DICOM study as a new series) in order to be properly managed and recalled. It may be appropriate to associate a series of JPEG images of a wound with the X-rays of the underlying broken bone, but in many cases, there is no formal DICOM study to which this type of informal imaging study can be associated. It is a standalone medical imaging study in its own right.
The ideal UniViewer application can accept, temporarily manage (if necessary) and display the non-DICOM images in their native format and therefore treat the set of images as an independent study.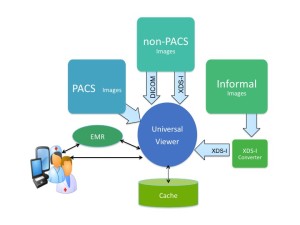
The question is, how are these images acquired from the capturing device, assembled into a formal study, and how is the appropriate metadata that identifies the patient, the study, and describes the study type created and associated with the study? Should this “acquisition application” be associated with the UniViewer, perhaps the VNA, or an enterprise workflow application? Is there an argument for it existing as a freestanding application? Regardless the source or configuration of the application, a methodology for creating an informal imaging study comprised of non-DICOM image objects should be a component of a healthcare organization’s strategy for image-enabling the EMR, because the clinicians will argue that they need access to the patient’s complete Medical Record, which should contain all of the clinically relevant images, not just radiology and cardiology.